In Ghana, the ‘Golden Minute’ Means Everything
Project HOPE’s trainings are empowering midwives across Ghana to save newborn lives when every second counts.
The delivery room fell silent. A newborn had just been born but was not breathing. For a moment, the mother’s joy hung in the balance.

Felicia A. Ankobil, a young midwife at Techiman Holy Family Hospital in Ghana’s Bono East Region, was ready. She had only recently completed the Helping Babies Survive/Essential Newborn Care training organized by Project HOPE’s Integrated Health Partnership, in collaboration with the Ghana Health Service and the Christian Health Association of Ghana.
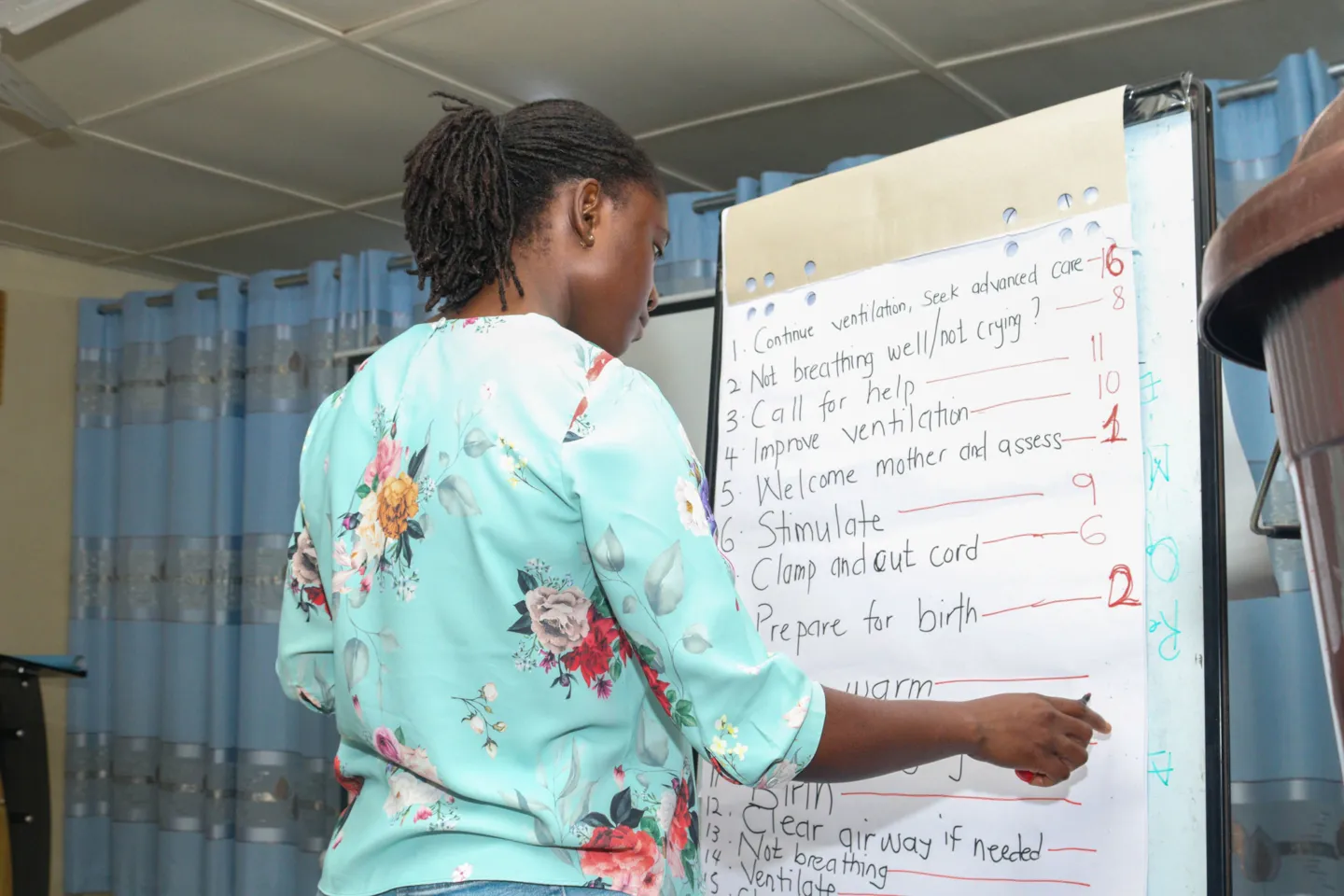
Because she had prepared her equipment at the start of her shift, Felicia calmly followed the steps she had practiced: dry thoroughly, stimulation, warmth, bag-and-mask ventilation. Within the “golden minute” — the first 60 seconds of life — the baby gasped and let out a cry. Relief filled the room.
“Previously, I might have waited too long or felt unsure,” Felicia said. “But this time, I sprang into action. That moment confirmed how powerful this training really is.”
For Felicia, saving a newborn was more than a clinical success. It was a gift. “Knowing that I can help a newborn take their first breath is humbling and fulfilling,” she said. “It is not just a skill — it’s a gift I can now offer to families in their most critical moments.”
And the results speak for volumes: since the training in June, Felicia and her team delivered 225 babies between August and September, successfully resuscitating 16 newborns.
From Learner to Trainer
When Felicia was selected to attend the training, she was surprised but proud. “I was very excited and honored,” she said. “I am still quite junior, so it felt like a big responsibility, but also a great opportunity to grow professionally and contribute more meaningfully to reducing newborn deaths.”
Before the training, she often faced emergencies without a clear roadmap. “I often saw situations where a newborn’s life hangs in the balance, and yet my knowledge to help was limited,” she said. “This training gave me confidence and the tools to act swiftly and correctly, which can make all the difference.” What stood out most was neonatal resuscitation. Hands-on practice during simulations helped transform theory into well-practiced routine. “Seeing how quickly things can turn critical, and knowing that a mother is counting on me, really hit me emotionally,” she said. “It made me realize how many lives could be saved if every health worker had this training.”
“It made me realize how many lives could be saved if every health worker had this training.”
Multiplying the Impact

Felicia’s role did not end with her own practice. As a trainer, she has already passed on lifesaving skills to 26 health workers across her facility and nearby clinics. “The greatest change I look forward to is seeing a significant drop in newborn deaths due to preventable causes,” she said. “I also want to see a culture shift, where every health worker prevents infection, provides respectful care, and feels empowered to act immediately.”
That shift is already visible. Muniratu Abubakari, one of the midwives Felicia trained, remembers how different things were before. “I often felt unsure and afraid when a newborn was in distress,” she said. “Sometimes I would wait for a more experienced colleague. It was heartbreaking to see a baby struggling and feel helpless because I did not know how to respond.”
Now, she says, the change is profound. “Recently, I resuscitated a baby who was not breathing, and within minutes, the baby cried,” she said. “It was incredibly rewarding to see the training in action.”
One exercise during the training transformed her outlook. “Seeing how quickly a coordinated, well-practiced team effort could bring a baby to life made me realize how critical every second is,” she said. “It also reminded me that even in high-stress situations, compassion and clear communication are just as vital as clinical skills.”
Through Felicia’s mentorship, every trained colleague becomes another link in a growing chain of life savers.
The Bigger Picture

Felicia’s story is part of a broader national effort led by Project HOPE through the U.S. Government-funded Integrated Health Partnership. The five-year initiative aims to reduce preventable maternal, newborn, and child deaths by improving access to quality care, strengthening health systems, and tackling persistent threats such as malnutrition, malaria, and antimicrobial resistance.
The need could not be more urgent. Nearly 40 of every 1,000 children in Ghana die before their fifth birthday, with most deaths occurring within the first month of life. Preventable causes such as birth asphyxia, prematurity, infections, and delays in care remain the leading causes. In 2024 alone, 5,667 out of 156,630 babies born in 61 high-volume facilities in Ghana required resuscitation. Birth asphyxia remains one of the leading causes of neonatal deaths — yet it is largely preventable when health workers are trained and equipped to act within the golden minute.
To address this challenge, Project HOPE and partners are scaling up Helping Babies Survive and Essential Newborn Care trainings, which focus on immediate and continued care of newborns from birth through the first month. The trainings emphasize hands-on, simulation-based trainings in resuscitation, thermal care, feeding, and early identification of danger signs.
In June and July 2025, Project HOPE conducted a five-day training-of-trainers for 28 master trainers from 14 regions: seven doctors, nine nurse specialists, and twelve midwives. Each region now has at least two trainers to cascade lifesaving skills to facility-level providers. The training combined simulations, group discussions, and Objective Structured Clinical Examinations (OSCEs) to strengthen skills in neonatal resuscitation, infection prevention, emergency preparedness, and family-centered care, while also preparing participants to train others.
The impact is clear: six graduates, including Felicia, have already cascaded the training to 83 frontline workers, with 72 more expected in the next round. This cascading model creates a powerful multiplier effect where one trainer equips dozens of colleagues, who then save lives daily in delivery rooms and neonatal wards across Ghana.
By embedding the trainings within national priorities, Project HOPE is ensuring local ownership, sustainability, and alignment with broader maternal and newborn health strategies. The initiative directly supports Project HOPE’s goal of reducing barriers to quality care and contributes to Sustainable Development Goal 3: Good Health and Well-being.
Looking Ahead
Felicia’s journey reflects the heart of Project HOPE’s mission: equipping frontline health workers with the skills, confidence, and support to save lives. Now, she approaches her work with hope — and it all begins with moments like that silent delivery room, when a baby’s first cry is heard within the golden minute, thanks to a midwife who was trained, ready, and empowered.
For Felicia, saving a newborn’s life is a gift of hope for families and communities. Through the Integrated Health Partnership, Project HOPE and partners are ensuring no mother loses a child to preventable causes, and that every baby has the healthiest possible start.
“I believe we will see healthier babies, more confident health workers, and stronger trust between communities and health facilities,” Felicia said. “Ultimately, this will contribute to lower newborn deaths and a stronger health system.”



